Millions of individuals globally suffer from diabetes, a chronic metabolic illness marked by increased blood glucose levels. Diabetes management is a challenging endeavor that calls for regular patient education, lifestyle changes, medication delivery, and close observation to avoid complications. The engagement of a multidisciplinary team (MDT) is essential in delivering complete and efficient patient treatment due to the complex nature of diabetes care. This article examines how important interdisciplinary teams are to improving diabetes patients’ care.
Recognizing Multidisciplinary Teams in the Management of Diabetes
When it comes to diabetes care, a multidisciplinary team usually consists of medical experts from different specialties who work together to handle the patient’s varied needs. Endocrinologists, primary care doctors, diabetes educators, nutritionists, nurses, pharmacists, and occasionally psychologists or social workers make up the core group. Every team member contributes a different set of abilities and expertise, resulting in a comprehensive strategy for managing diabetes.
The Advantages of a Diverse Strategy
Comprehensive Patient Care:
Enabling comprehensive patient care is one of the main advantages of a multidisciplinary approach. Diabetes affects several bodily systems, thus managing it calls for knowledge in a variety of medical specialties. A nutritionist offers advice on nutrition and meal preparation, while an endocrinologist is concerned with controlling blood sugar levels and medicine. A diabetes patient care educator assists in comprehending the illness, its consequences, and the best ways to successfully monitor their health. This cooperative method guarantees that every facet of a patient’s treatment is attended to.
Individualized Treatment Plans:
The management of diabetes necessitates customized treatment plans that take into account each patient’s unique requirements, preferences, and lifestyle. By combining their knowledge, a multidisciplinary team can develop a treatment plan that is more unique to each member. A dietician may create a meal plan specific to the patient’s cultural preferences, a pharmacist might spot possible prescription interactions, and a nurse could instruct on administering insulin. Better results and increased adherence to therapy are possible with this individualized care.
Better Patient Education and Self-Management:
One of the main pillars of diabetes care is education. It is important for patients to know about their condition, how to treat it, and how to avoid consequences. A multidisciplinary team that addresses different facets of diabetes management might provide more thorough instruction. For instance, a psychologist could assist patients in managing the emotional difficulties associated with having a chronic illness, while a diabetes educator might instruct patients on how to check their blood glucose levels. Patients who have had a good education are more likely to practice self-management skills, which are essential for long-term success.
Improved Care Coordination:
Individuals with diabetes frequently need care from several different medical professionals, which, if not properly coordinated, can result in fragmented care. A multidisciplinary team makes it easier for healthcare professionals to coordinate and communicate with one another, resulting in seamless patient care. By working together, we can increase patient safety by lowering the possibility of medical errors like redundant testing or incompatible treatment regimens.
Early Complications Identification and Prevention:
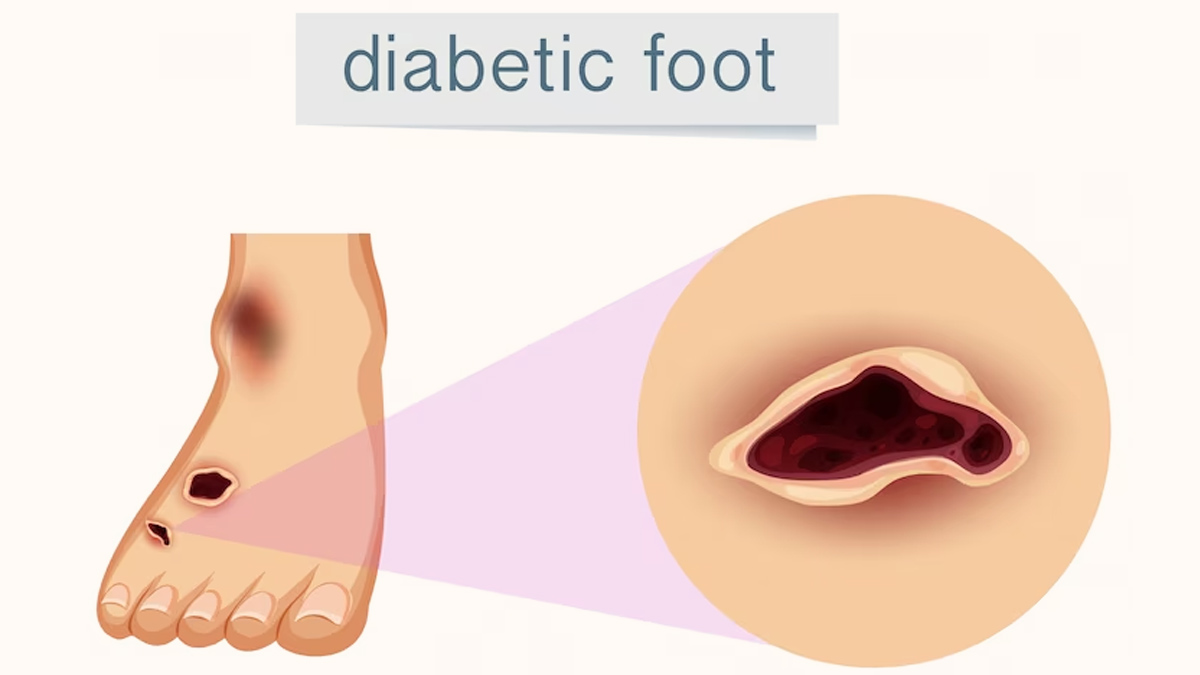
Diabetes may cause major side effects such as retinopathy, renal failure, neuropathy, and cardiovascular disease. Improving patient outcomes requires the early detection and prevention of these problems. A multidisciplinary team can monitor patients more efficiently and see possible issues before they become serious. For example, a nephrologist may diagnose kidney problems before they proceed to renal failure, while an ophthalmologist may recognize the early indicators of diabetic retinopathy. The quality of life for the patient can be improved by early intervention, which can also postpone or avoid the start of problems.
Support for Behavioral and Mental Health:
Although it is sometimes disregarded, the psychological effects of having diabetes have a big influence on how well patients turn out. Patients frequently experience diabetes distress, anxiety, and depression, all of which can have a detrimental impact on medication adherence and self-management. For these problems, a multidisciplinary team with mental health specialists on board can offer assistance. Through addressing the psychological and emotional components of diabetes, the team can assist patients in keeping a positive attitude and continuing to participate in their care.
Empowerment and Patient-Centered Care:
By including patients in decision-making and offering them assistance from a variety of sources, a multidisciplinary team approach empowers patients. Patients who receive care from a team that takes into account all facets of their well-being report feeling more understood and supported. The patient’s values, preferences, and wants are respected under this patient-centered care model, which improves overall health outcomes and patient satisfaction.
Obstacles and Prospects for the Future
Although the advantages of multidisciplinary teams in the treatment of diabetes are obvious, there are obstacles to overcome in order to successfully apply this strategy. It can be challenging for team members to coordinate, particularly in healthcare institutions where communication is compartmentalized. Furthermore, not every healthcare environment has the funding necessary to maintain a fully interdisciplinary staff.
In the future, technology has a big part to play in addressing these obstacles. Electronic health records, patient management software, and telemedicine can help team members communicate and work together more effectively. In addition, it is imperative for healthcare systems to give precedence to the education and training of interdisciplinary teams in order to guarantee that every patient receives comprehensive care.
In summary
In order to address the multifaceted needs of diabetes, multidisciplinary teams offer a comprehensive, patient-centered approach that is crucial in managing the condition. These teams can provide comprehensive care, individualized therapy, and support for self-management by combining the knowledge of many healthcare providers, which will ultimately improve patient outcomes. Multidisciplinary teams will play a bigger and bigger role in providing patients with diabetes with high-quality care as healthcare continues to change.