Overview
Antibiotics have completely changed the way bacterial infections are treated, giving medical personnel essential tools to fight against a wide range of pathogens. Of these antibiotics, Cephalexin—also marketed under the name Keflex—is one that is often administered. It is crucial for patients and medical professionals to know how Cephalexin stacks up against other antibiotics. The unique qualities of Cephalexin, its efficacy, and its position within the larger framework of antibiotic therapy are all examined in this article.
An overview of cephalexin
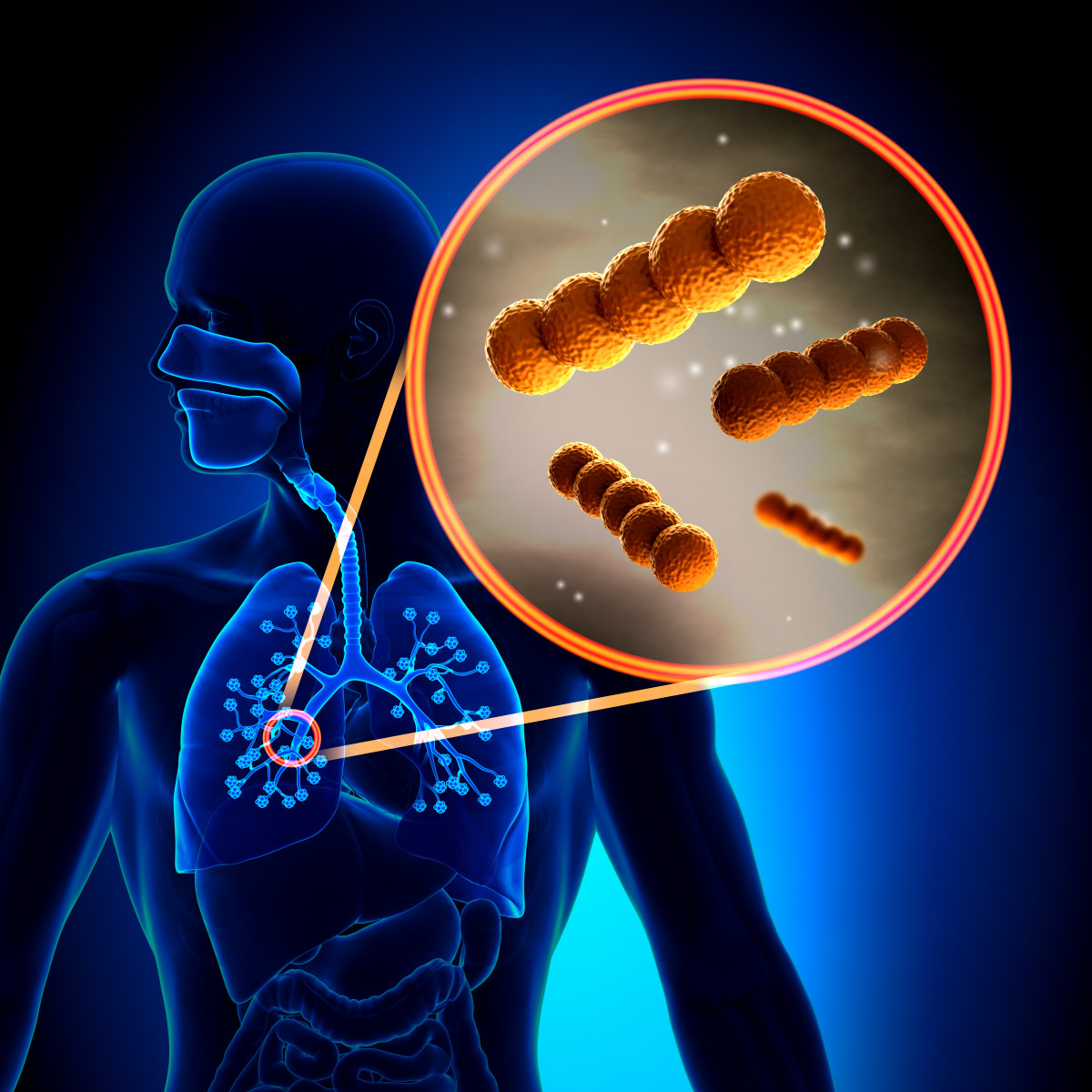
The antibiotic class that includes cephalexin is called cephalosporin. A class of beta-lactam antibiotics known as cephalosporins prevent the formation of bacterial cell walls, which kills the bacterium. As a first-generation cephalosporin, cephalexin works well against a variety of gram-positive and certain gram-negative bacteria.
Mechanism of Action:
The bacterial cell wall contains penicillin-binding proteins (PBPs), which are bound by cephalexin. The bacterial cell wall’s essential component, peptidoglycan, is inhibited by this interaction, which eventually causes cell lysis and death.
Indications:
Common infections that cephalexin keflex is used to treat include:
infections of the skin and soft tissues
infections of the respiratory system
Ear infections, or otitis media
bone infections
UTIs, or urinary tract infections
Dosage and Administration:
Cephalexin comes in capsule, tablet, and liquid suspension forms and is usually taken orally. The patient’s age, general health, and the type of infection being treated all affect dosage. It is typically taken every 6 to 12 hours in doses between 250 and 500 mg.
Comparing This Antibiotic with Others
It’s helpful to compare Cephalexin to other antibiotic classes, such as penicillins, macrolides, fluoroquinolones, and tetracyclines, in order to comprehend how it differs from these others.
Penicillins
Penicillin is a beta-lactam antibiotic and one of the first to be identified. It functions by preventing the formation of bacterial cell walls, just like cephalexin. Penicillin works especially well against a variety of gram-positive bacteria, such as species of Staphylococcus and Streptococcus.
Benefits of Cephalexin over Penicillin:
Cephalexin is more effective against certain gram-negative bacteria than Penicillin may be, and it has a wider range of activity. Furthermore, individuals who are tolerant of cephalosporins yet allergic to penicillin are frequently treated with cephalexin.
Limitations:
Although there is little cross-reactivity between penicillin and cephalosporins, both cephalexin and penicillin have the potential to cause allergic responses. Beta-lactamase-producing bacteria can reduce the effectiveness of penicillin, and these enzymes can also damage cephalexin.
Macrolides
Another class of antibiotics known as macrolides, which bind to the 50S ribosomal subunit to prevent bacterial protein production, includes azithromycin and clarithromycin. They are frequently applied to atypical pathogens and respiratory diseases.
Benefits of Cephalexin over Macrolides:
Because of its broad-spectrum activity against both gram-positive and gram-negative bacteria, Cephalexin may be chosen for certain infections. Comparatively speaking, it is also less likely to be implicated in drug interactions than macrolides, which can disrupt other medications’ cytochrome P450 system-mediated metabolism.
Cons:
Cephalexin does not protect against atypical organisms such as Mycoplasma pneumoniae and Chlamydia pneumoniae, which macrolides are effective against. The efficacy of cephalexin in treating various kinds of infections might be restricted.
Fluoroquinolones
The broad-spectrum antibiotics known as fluoroquinolones, which include ciprofloxacin and levofloxacin, function by preventing the bacterial enzymes topoisomerase IV and DNA gyrase, which are necessary for DNA replication.
Benefits of Cephalexin over Fluoroquinolones:
Because of its safety record and decreased potential to cause resistance, Cephalexin is frequently chosen for treating simple infections. The use of fluoroquinolones may be restricted in certain patients due to their notable adverse effects, which include tendon injury and QT prolongation.
Cons:
While Cephalexin does not address Pseudomonas aeruginosa, fluoroquinolones have a wider range of activity and are more efficient against gram-negative bacteria in general. In cases where Cephalexin may not be adequate, they are also helpful in treating complex infections.
tetracyclines
Tetracyclines bind to the 30S ribosomal subunit and prevent bacterial protein production. Examples of these compounds are minocycline and doxycycline. They work well against several unusual infections as well as a broad variety of bacteria.
The usage of cephalexin is more widespread than tetracyclines due to its effectiveness in treating common bacterial infections. It is also often better tolerated due to its adverse effect profile, which is generally better than tetracyclines’, which can include gastrointestinal disturbances and photosensitivity.
Cons:
Tetracyclines are more effective against intracellular infections including Chlamydia and Rickettsia, and they have a wider range of activity. These pathogens are not covered by cephalexin.
Safety Profile and Resistance
Antibiotic Resistance:
The emergence of antibiotic resistance is one of the main issues with antibiotic therapy. Like other antibiotics, cephalexin might cause resistance if it is not taken as directed. Cephalexin’s efficacy can be diminished by misuse or overuse, which can result in the emergence of bacterial strains that are resistant to it.
Safety Profile:
Generally well-tolerated, cephalexin might cause gastrointestinal symptoms such nausea, vomiting, and diarrhea as common side effects. There may be allergic responses or infrequent cases of anaphylaxis. When compared to certain other antibiotics, especially the fluoroquinolones, which have more severe side effects, its safety profile is generally better.
Clinical Points to Remember
Selecting the Appropriate Antibiotic:
The selection of an antibiotic is contingent upon various criteria, such as the nature of the infection, the bacteria responsible, the patient’s allergies, and any possible adverse reactions. Cephalexin is frequently used due to its good safety profile and efficacy against common gram-positive infections.
Patient Factors:
Because cephalexin is excreted by the kidneys, dose modifications may be required in patients with renal impairment. When administering Cephalexin, it is imperative to take into account any prior history of allergies to cephalosporins or penicillins.
In summary
Among antibiotics, cephalexin is unique in that it works well against a variety of gram-positive and some gram-negative bacteria, making it a useful treatment for a number of infections. It has limitations and isn’t always the best option for all infections, even while it has certain advantages over other classes of antibiotics, such as its safety profile and spectrum of activity. By being aware of these subtleties, medical personnel may improve antibiotic therapy and make well-informed decisions, which ultimately improves patient outcomes and helps tackle the rising problem of antibiotic resistance.