Non-Surgical Incontinence Treatment: Empowering Solutions for Improved Quality of Life
Introduction: Urinary incontinence is a common and often distressing condition that affects millions of individuals worldwide. While traditional treatment options such as medication and surgery have been available, non-surgical approaches have emerged as effective alternatives for managing incontinence. In this article, we explore the various non-surgical treatment options for urinary incontinence, their benefits, and how they can empower individuals to regain control over their https://direct-ui.com/about-us/ function and quality of life.
Understanding Urinary Incontinence: Urinary incontinence refers to the involuntary leakage of urine, which can occur due to various factors such as weakened pelvic floor muscles, nerve damage, hormonal changes, or underlying medical conditions. It can manifest in different forms, including stress incontinence (leakage during physical activity), urge incontinence (sudden, intense urge to urinate), or mixed incontinence (combination of stress and urge incontinence). Regardless of the type, urinary incontinence can significantly impact an individual’s confidence, social activities, and overall well-being.
Non-Surgical Treatment Options: Non-surgical treatment options for urinary incontinence aim to address underlying causes, strengthen pelvic floor muscles, and improve bladder control without the need for invasive procedures. Some of the most common non-surgical treatments include:
- Pelvic Floor Exercises (Kegels): Pelvic floor exercises, also known as Kegels, involve contracting and relaxing the muscles of the pelvic floor to strengthen them over time. These exercises can help improve bladder control, reduce urinary leakage, and enhance pelvic floor muscle tone. They are often recommended as a first-line treatment for stress incontinence and can be performed discreetly at home or under the guidance of a pelvic floor physiotherapist.
- Bladder Training: Bladder training involves gradually increasing the intervals between urination to help train the bladder to hold larger volumes of urine and reduce the frequency of urinary urgency and leakage. This technique may include scheduled voiding times, delayed voiding when the urge to urinate arises, and relaxation techniques to manage urgency sensations. Bladder training can be highly effective for individuals with urge incontinence or overactive bladder.
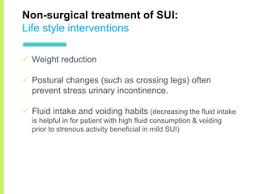
- Lifestyle Modifications: Certain lifestyle factors can exacerbate urinary incontinence symptoms, such as caffeine consumption, smoking, alcohol intake, and excessive fluid intake. Making lifestyle modifications, such as reducing caffeine and alcohol consumption, maintaining a healthy weight, and practicing good toilet habits, can help alleviate symptoms and improve bladder control.
- Pelvic Floor Electrical Stimulation: Pelvic floor electrical stimulation involves the use of electrical currents to stimulate and strengthen the pelvic floor muscles. This treatment may be delivered via vaginal or anal probes or external electrodes placed on the skin. Electrical stimulation can help improve muscle tone, reduce urinary leakage, and enhance bladder control, particularly in individuals with weak pelvic floor muscles.
- Biofeedback Therapy: Biofeedback therapy utilizes specialized equipment to provide real-time feedback on pelvic floor muscle activity and bladder function. This visual or auditory feedback helps individuals learn how to properly contract and relax their pelvic floor muscles, improve bladder control, and reduce urinary incontinence episodes. Biofeedback therapy is often used in conjunction with pelvic floor exercises to enhance their effectiveness.
Benefits of Non-Surgical Treatment: Non-surgical treatment options for urinary incontinence offer several benefits for individuals seeking to regain control over their bladder function and improve their quality of life. Some of the key benefits include:
- Non-Invasive: Non-surgical treatments do not require incisions, anesthesia, or recovery time, making them suitable for individuals who prefer to avoid surgery or are not candidates for surgical intervention.
- Cost-Effective: Non-surgical treatments are generally more cost-effective than surgical procedures, making them accessible to a broader range of patients.
- Customized Approach: Non-surgical treatment plans can be tailored to each individual’s specific needs, symptoms, and preferences, allowing for personalized care and optimal outcomes.
- Improved Quality of Life: By reducing urinary leakage, enhancing bladder control, and empowering individuals to manage their symptoms effectively, non-surgical treatments can significantly improve quality of life and overall well-being.
Conclusion: Urinary incontinence is a prevalent condition that can have a profound impact on an individual’s daily life and emotional well-being. Non-surgical treatment options offer effective, accessible, and empowering solutions for managing urinary incontinence and improving bladder control. By incorporating pelvic floor exercises, bladder training, lifestyle modifications, and other non-invasive techniques into a comprehensive treatment plan, individuals with urinary incontinence can regain confidence, independence, and a higher quality of life. It is essential for individuals experiencing urinary incontinence to consult with a healthcare professional to determine the most appropriate treatment approach based on their specific needs and circumstances.